Researchers studying gut bacteria and the brain have made some interesting discoveries. This article looks at how gut bacteria might be connected to certain disorders such as depression and anxiety.
Welcome, reader, to another installment in our series exploring the role of intestinal bacteria in the health of our brains. In another article, we examined the “gut-brain axis.” In this article, we explore how the health of the residents of our digestive tracts—our gut bacteria and fungi—has a direct connection to our brain health. We look at how what we eat and drink affects our internal community (known as “gut flora” or “gut microbiome”). We also explore how important it is to keep it in tip-top shape for our overall well-being.
Many factors have an effect on our gut flora–not only what we ingest. How much we sleep, how stressed we are, and how often we take antibiotics all have an influence on the welfare of that hard-working community.
This area of science has become more popular in recent years. Because of this interest, researchers have performed many new studies looking into the connection between gut bacteria and the brain. Let’s take a look at some of those studies, and what they revealed.
Gut Bacteria and the Brain: The Tale of the Mournful Mice
In a study on mice published by French researchers in December 20201, researchers found that stress caused imbalances in the gut microbiome. In addition to these flora imbalances, scientists found that the animals who were stressed displayed symptoms similar to depression. These symptoms include reduced grooming, weight loss, and a reduction in the number of new brain cells being produced. One explanation for this is that stress might cause damage to the gut flora and this change in the microbiome led to depressive symptoms. Researchers found that one mechanism that caused some of these changes involved the Endocannabinoid system..
The endocannabinoid system
In this study, scientists found that the “depressed mice” were experiencing a decrease in “endocannabinoid signalling”. Endocannabinoid signals2—a recent area of scientific interest—are a system of neurotransmitters. These signals are implicated in important physiological and cognitive processes. These processes include mood, memory, appetite, fertility and the creation of new brain cells.
Where do these endocannabinoids come from? Our bodies make them. However, the bacteria in the gut play a role in regulating fatty acid metabolism and therefore the production of the raw materials needed to make Endocannabinoids. Fatty acids, as I discussed in another article, are highly beneficial to the health of your brain. Flax seeds, walnuts, and fatty fish are all great sources of healthy fatty acids for the brain, by the way!
In case you were wondering, endocannabinoids are linked to cannabis. In fact, the scientists who discovered the endocannabinoid system (ECS) were actually studying cannabis. They realized that a number of plant compounds could affect the ECS, but most notably THC and CBD in cannabis. The human body, however, does not need external input of cannabis or other plants. In fact, we synthesize endocannabinoids ourselves3. Pretty neat, huh?!
The results of the study
So anyway, back to the mice. Stress caused them to have reduced production of endocannabinoids. This led to symptoms of depression. This correlation made the researchers wonder if an imbalance in gut flora was causing the problem. A gut that can’t properly process nutrients can’t deal with those fatty acids and effectively make them into neurotransmitters (endocannabinoids).
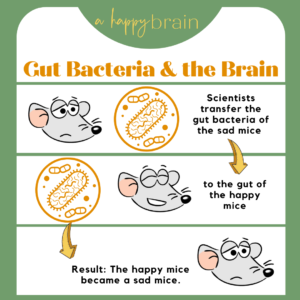
To study this idea, the researchers transplanted some of the bacteria from the stressed mice into a group of their super-chill, laid back cousins. This change in their gut microbiota soon caused the laid back to experience the same symptoms as the stressed mice. This change in demeanor showed that gut bacteria was having a clear effect on the mood of the host.
“Surprisingly, simply transferring the microbiota from an animal with mood disorders to an animal in good health was enough to bring about biochemical changes and confer depressive-like behaviors in the latter.” concluded Pierre-Marie Lledo4 – joint author of the study.
A Bacterial Explanation
So, what exactly was the difference in the colony of bacteria? Well, one of the major differences that the researchers discovered was that the stressed mice had reduced levels of the “Lactobacillus” bacteria5. To understand more, let’s take a look at that particular genus, and why scientists are taking a keen interest in its effect on brain health.
Bacteria predate us on this planet by billions of years, and are sure to outlive the human race. We have approximately 40 trillion bacteria in our intestinal tract. The majority of these belong to about 40 species (although we may have up to 1000 species, depending on the person).
Lactobacillus is a genus of bacteria comprising over 260 different species. They are the most common type of bacteria in the gut, and help us to digest the food we eat. In addition, they help protect against “bad” bacteria, and support our immune system.
Also known as “lactic acid bacteria” or simply “LAB”, they are also found in fermented foods. These fermented foods include yogurt, kombucha, and cheese. They are also commonly used in probiotic supplements. In line with the findings of the mouse experiment above, studies have found that human patients with depressive disorder have a lower count of lactobacillus6 than usual in their system.
Other research has also proven that LAB have an important role in human mood and mental health. One study7 showed how Lactobacillus helveticus and bifidobacterium led to fewer depressive symptoms and lower psychological stress in patients.
Researchers examined the effects of Lactobacillus rhamnosus in a study in 20178. In this study, scientists discovered that these bacteria have a surprisingly powerful influence on the mental health of their hosts. Doctors have used this strain of LAB to treat postpartum depression and anxiety. This treatment significantly decreases the severity of these conditions.
Lactobacillus casei, in particular the strain “shirota”, was found to help with dealing with stress9. This strain reduced the amount of cortisol produced, protecting the body from the negative side-effects of stressful situations.
Pretty impressive performance from a teeny-tiny bacteria, I think you’ll agree!
That’s it for today, as I feel that is a whole lot of information to digest(!). As you can see, the bacteria in our guts have a huge affect on the health of our brains. The gut-brain axis is a fascinating and complicated subject, and one which I will continue to explore in more detail in future articles. I look forward to seeing you there!
Dr. Annissa Slusher
References:
- https://www.nature.com/articles/s41467-020-19931-2
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3517813/
- https://www.sciencedirect.com/topics/neuroscience/endocannabinoids
- https://research.pasteur.fr/en/member/pierre-marie-lledo/
- https://www.sciencedirect.com/topics/food-science/lactobacillus
- https://www.sciencedirect.com/science/article/abs/pii/S0165032716302701
- https://www.cambridge.org/core/journals/british-journal-of-nutrition/article/assessment-of-psychotropiclike-properties-of-a-probiotic-formulation-lactobacillus-helveticus-r0052-and-bifidobacterium-longum-r0175-in-rats-and-human-subjects/2BD9977C6DB7EA40FC9FFA1933C024EA
- https://www.sciencedirect.com/science/article/pii/S2352396417303663
- https://www.nature.com/articles/tp201694

